Articles
ANKLE SPRAIN: OSTEOPATHIC TREATMENT
 One of the traumas that most frequently affects the body is the ankle sprain or ‘twisted ankle’. The most common injury is a sprain of the ligament(s) on the outer side of the ankle. Other common injuries include strain of a muscle/tendon on the outer side of the lower leg and fracture of the lower outer prominence of the leg bone. Ankle sprain may be more common in athletes than other patients, often when the foot is supinated or when there are some anatomical conditions such as a longer fibular malleolus or a stiffer deltoid ligament. It is also more frequent after a previous sprain, because of the joint instability.
One of the traumas that most frequently affects the body is the ankle sprain or ‘twisted ankle’. The most common injury is a sprain of the ligament(s) on the outer side of the ankle. Other common injuries include strain of a muscle/tendon on the outer side of the lower leg and fracture of the lower outer prominence of the leg bone. Ankle sprain may be more common in athletes than other patients, often when the foot is supinated or when there are some anatomical conditions such as a longer fibular malleolus or a stiffer deltoid ligament. It is also more frequent after a previous sprain, because of the joint instability.If untreated, ankle sprain may lead to:
- chronic pain in other parts of the same or opposite foot
- chronic pain elsewhere in the body, such as the knee, hip and/or lower back, due to altered gait (e.g. limping) from ankle pain.
Immediate treatment
Firstly, straight after an acute ankle sprain it is better to follow the mnemonic R.I.C.E.: Rest, Ice, Compression (bandage), Elevation.
Therapy
Osteopathy, physiotherapy, massage therapy, acupuncture and many other manipulative treatments are very crucial to tackle all the symptoms and dysfunctions related to the ankle. When treating ankle pain it is essential to examine the entire lower limb and the lower back because during weight bearing your foot is part of a closed mechanical chain.
The joint alteration that involves a sprained ankle is generally non-permanent: the treatment aims to treat bones, joints, ligaments, muscles, tendons, nerves and circulation, making the rehabilitation easier.

Osteopathy
The osteopathic treatment reduces the local joint stiffness, the tightness of muscles, tendons and ligaments (for example, the talofibular ligament). Often crucial, it is important to treat the whole leg and the interosseous membrane, to improve nerves and circulation. The osteopath will also check and treat the rest of the body, especially all the mechanical connections such as the hip, the sacrum (SI joint as well), the spine, and the relevant soft tissues. Most of the time a proper taping is used to facilitate the recovery, support of the joint and to treat the swelling.
Long term resolution can be achieved by identifying and managing underlying causative and maintaining factors.
Written by Fabio Basile
Jaw disorders, Headache, Neck pain and… Osteopathy!
 Is your jaw causing you pain, tension, clicking, clenching or grinding? Jaw muscles and the actual joint (temporo-mandibular joint/TMJ) consist of hard and soft tissue structures (e.g. joint surfaces, capsule, articular disk, ligaments, masticatory muscles). Masticatory muscles are responsible for all movements of the jaw, allowing a number of functions such as chewing, sucking and swallowing, articulating sounds, breathing, and making facial expressions. The jaw works properly when the right-sided and left-sided joints are synchronized during movement.
Is your jaw causing you pain, tension, clicking, clenching or grinding? Jaw muscles and the actual joint (temporo-mandibular joint/TMJ) consist of hard and soft tissue structures (e.g. joint surfaces, capsule, articular disk, ligaments, masticatory muscles). Masticatory muscles are responsible for all movements of the jaw, allowing a number of functions such as chewing, sucking and swallowing, articulating sounds, breathing, and making facial expressions. The jaw works properly when the right-sided and left-sided joints are synchronized during movement. Symptoms may include:
- clicking, clenching or grinding within the joint
- mechanical restrictions (e.g. limited jaw opening capacity, deviations in the movement patterns of the mandible)
- stiffness
Osteopathic treatment can help to improve the mechanics and tension to reduce your symptoms and reduce tension. Osteopathy is a physical therapy intervention, characterized by fine manipulative techniques, individually adapted to tissue quality, in order to maintain or restore the function of numerous body structures. These interventions are commonly used to reduce pain and to improve mandibular range of motion. Absence of pain, improved TMJ function, and normal quality of life are appropriate markers of treatment success.
Headache and Neck pain
The TMJ makes muscular and ligamentous connections to the cervical region, forming a functional complex called the cranio-cervico-mandibular system. The TMJ/Jaw can often link to other problems in the body such as headaches and neck pain. If you are experiencing those symptoms your Osteopath will assess your jaw to rule out or treat any link between these disorders.
Example of treatment: TMJ ligaments and muscles

Osteopathic treatment in this area can be of great help in returning balance to the body posture. A complete protocol includes treatment of different body sites, such as: thoracic and cervical spine, neck muscles and viscera, cranial bones and muscles.
TMJ ligaments’ treatment: specific manipulative techniques for accessory ligaments of the temporomandibular joint, including the sphenomandibular, stylomandibular, and pterygomandibular ligaments. These techniques are designed to reduce ligament dysfunction and to retrain the involuntary neuromuscular, reflexive control of posture and balance.
TMJ muscles’ treatment: application of neuromuscular technique over trigger points in the masseter and temporal muscle. It induces a decrease in pressure pain sensitivity and an increase in active mouth opening.
Written by Fabio Basile
Get ready for London Marathon: Hip, ‘toe’…hooray!
Going the distance and running your marathon or half-marathon this year? Long distance running puts your legs (from hip to toe) through the wringer.

Before to cheer, saying ‘Hip, hip hooray’, you hopefully would have started a good training few months ago to ensure a safe progression. A challenge like the marathon is incredibly rewarding but also very tough on the body. Increasing your exercise capacity to this level pushes the limits of endurance both physically and mentally. Training for long races, which of course includes, long runs, puts a lot of stress on the muscles and tendons of your legs. Get the most mileage out of your lower half with expert tips to keep your legs in tip-top shape throughout training and, of course, through race day.
As you ramp up your mileage in training, your muscles and posture are more apt to dysfunctions and adaptations which lead to postural imbalance and result in soreness and pain. Muscles that typically need a little extra consideration during long race training are hip muscles, quads, hamstrings, and calves (see below ‘don’t forget to stretch’ for further details).
EXPERT-BACKED TIPS
- Active rest and recovery: your old friend "rest day" is the fix! Furthermore, sleeping! That is underestimated as a tool for recovery. This is when your body can shut down and truly rebuild.
- Diet: eat balanced meals and stay hydrated, it's very common for marathon runners to be unknowingly dehydrated during training.
- Compression: research suggests compression (socks, sleeves, etc.) might increase blood flow to the heart, helping clear muscular waste products, such as lactic acid, that make your legs feel like lead after a long run.
- Cross-Train: don't forget your other recovery tools to keep your legs in shape throughout training and race day. Non-impact cross training like swimming, cycling, and using the elliptical make for smart active recovery.
- Don't forget to stretch: stretching and foam rolling when your body is still warm from your workout will help loosen tight muscles. You should do it after every run, focusing on every crucial muscle, even the unimaginable! For example, hip flexion is controlled by quads, psoas and sartorius, which plays an important role in hip motion and, consequently, some unclear pain around the hip. Don’t miss piriformis, hamstrings, gastrocnemius, soleus, tibialis anterior, also stretching and considering your feet posture.
- Osteopathy and Sports massage: see below…
HOW OSTEOPATHY AND MASSAGE THERAPY CAN HELP IN THE RUN UP TO THE LONDON MARATHON.
We can assess and correct your postural symmetry and length-tension relationship of the muscles, both running and in general. For example, most people favour one side of their body and lean a little. This may not cause issues in everyday life (although it often can) but when putting the body through lots of miles, both during the race and in training, a small imbalance can develop into far more painful and debilitating problems.
Even without problems, a good muscular and joint mobility treatment can be very beneficial during training, especially when tightness has started to develop.
Written by Fabio Basile
Shoulder pain, pectoralis muscle and…Weight training
 The anatomy of the shoulder is based on complex joint biomechanics, which guarantee the coexistence of both maximum mobility and stability within the same joint. The bone structures inside the shoulder include the humerus, the scapula, the acromion process, the clavicle, the greater tubercle, and the glenoid cavity. The Rotator Cuff muscles are connected individually to a group of flat tendons, which fuse together and surround the front, the back, and the top of the shoulder joint like a cuff on a shirt. The tendons attach the muscles to the bone and allow movement in the shoulder, as well as providing strength to hold the ball in its socket. These tendons are called the subscapularis tendon, the supraspinatus tendon, the infraspinatus tendon, and the teres minor tendon.
The anatomy of the shoulder is based on complex joint biomechanics, which guarantee the coexistence of both maximum mobility and stability within the same joint. The bone structures inside the shoulder include the humerus, the scapula, the acromion process, the clavicle, the greater tubercle, and the glenoid cavity. The Rotator Cuff muscles are connected individually to a group of flat tendons, which fuse together and surround the front, the back, and the top of the shoulder joint like a cuff on a shirt. The tendons attach the muscles to the bone and allow movement in the shoulder, as well as providing strength to hold the ball in its socket. These tendons are called the subscapularis tendon, the supraspinatus tendon, the infraspinatus tendon, and the teres minor tendon. 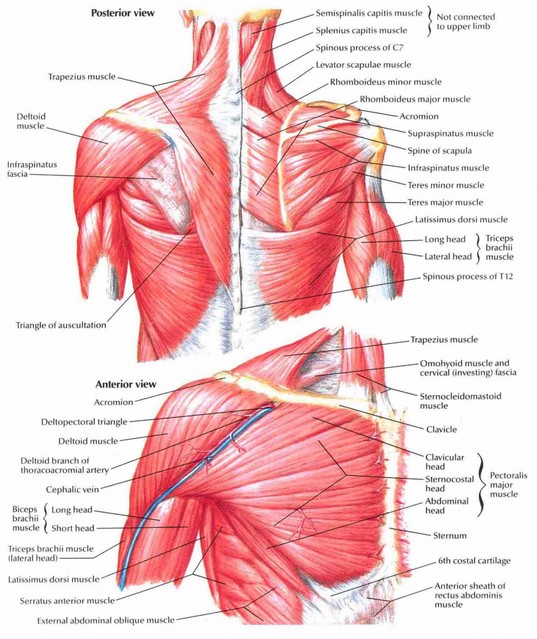 Other main muscles (and tendons) in the shoulder area include: biceps, pectoralis minor, deltoids, subclavius, trapezius, teres major, serratus anterior sternocleidomastoid, levator scapulae, rhomboids. The tendons are the most vulnerable part of the shoulder and is where most shoulder injuries occur.
Other main muscles (and tendons) in the shoulder area include: biceps, pectoralis minor, deltoids, subclavius, trapezius, teres major, serratus anterior sternocleidomastoid, levator scapulae, rhomboids. The tendons are the most vulnerable part of the shoulder and is where most shoulder injuries occur.Biceps and Pectoralis muscles
Between the biceps and the pectoralis minor there is a relationship, together with a third structure, such as the brachial nerve. A mechanical imbalance (strength or weakness, bad posture, overtraining) can generate a painful and/or hypofunctional sensation. When the biceps and/or pectoralis are in this situation, the patient can report anterior shoulder pain, focused on a specific area (anterior shoulder) or radiating along the biceps brachii muscle, which often involves the brachial nerve.
Weight training
Weight training forms a standard fitness regimen in many sports. A high incidence of shoulder injuries has been reported in weightlifting, bodybuilding, crossfit and functional training. Within the shoulder, tendinopathies of the rotator cuff, long head of biceps and pectoralis major muscle have been described as complications of weight lifting.
The Bench-Presser’s Shoulder
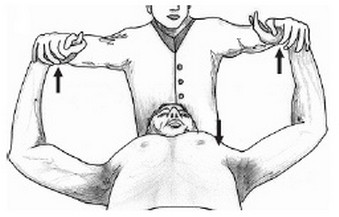
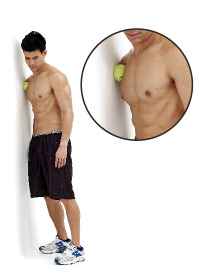
Insertional tendinopathy of pectoralis minor is an undescribed cause of shoulder pain in weightlifters or sportsmen. This condition is described as ‘‘Bench-Presser’s Shoulder’’. Pectoralis minor tendon is the only significant structure that inserts on the medial surface of the coracoid process (front of the shoulder). Pain resulting from the active contraction test (see picture) and the press exercises, both of which result in contraction of pectoralis minor, also suggests an inflammation of the above-mentioned tendon.
Risky exercises (whether there’s an issue about strength or weakness, bad posture, overtraining):
- Bench press (bar or dumbbells)
- Chest press
- Push-ups
- TRX (chest press)
- Burpees (because of push-ups)
IMPORTANT: even training chest and biceps in the same session can increase the risk of feeling pain (think about the correct split routine!).
What to do:
- Stop doing the “risky exercises”
- Have the right consultation with a professional practitioner to improve joint mobility and tackle the stiffness, tightness and tenderness
- Stretch it gently
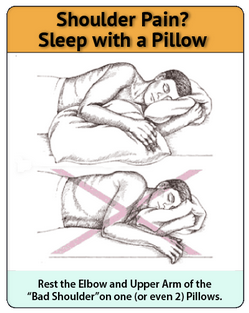
- Sleep properly (see picture)
Stretching-Release:
- EX 1: Myofascial release with a tennis ball against the wall

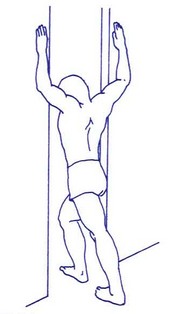
- EX 2: Pectoralis muscle stretching against a corner or a door frame
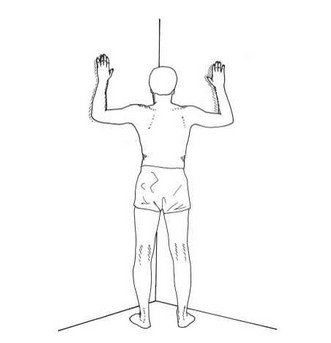
- EX 3: Relaxing posture (laying down, legs against the wall, arms straight and relaxed on the ground)

Written by Fabio Basile
‘Text neck’ and Osteopathy
 In our digital society, the use of smartphones has increased rapidly. Parallel with the growing use of smartphones, musculoskeletal problems associated with intensive smartphone use have also increased. Recent investigations showed that mobile device users tend to report pain symptoms on the neck, shoulder and thumb, and the severity of the symptoms increased with the total time spent using their mobile devices. Neck flexion is the most commonly adopted posture by smartphone users while looking at the visual display terminals of smartphones for extended periods; this posture may lead to neck disorders.
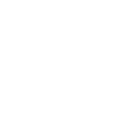
In our digital society, the use of smartphones has increased rapidly. Parallel with the growing use of smartphones, musculoskeletal problems associated with intensive smartphone use have also increased. Recent investigations showed that mobile device users tend to report pain symptoms on the neck, shoulder and thumb, and the severity of the symptoms increased with the total time spent using their mobile devices. Neck flexion is the most commonly adopted posture by smartphone users while looking at the visual display terminals of smartphones for extended periods; this posture may lead to neck disorders.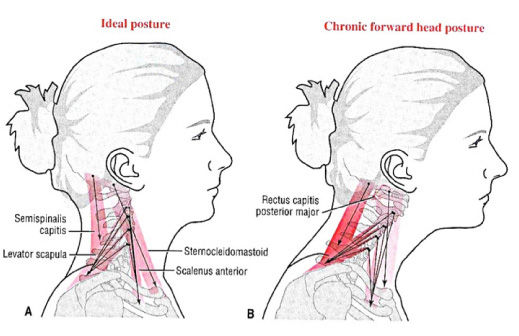 Pain in the neck of smartphone users, which has often been referred to ‘text neck’ (also called 'tech neck'), has received more public attention recently due to the growing use of mobile devices in head forward flexion postures [Figure]. Smartphone users typically hold the device using one or two hands below their eye height, look down at the device and type or touch the touch-screen display mostly using the thumb. Physical stresses on the neck and resultant health concerns associated with the frequent and/or prolonged head flexion have been frequently studied previously in research about the position of personal computer (PC) displays. Placing a computer display too high or low is known to cause awkward postures of the user and produce neck muscle fatigue and discomfort after a prolonged period of use.
Pain in the neck of smartphone users, which has often been referred to ‘text neck’ (also called 'tech neck'), has received more public attention recently due to the growing use of mobile devices in head forward flexion postures [Figure]. Smartphone users typically hold the device using one or two hands below their eye height, look down at the device and type or touch the touch-screen display mostly using the thumb. Physical stresses on the neck and resultant health concerns associated with the frequent and/or prolonged head flexion have been frequently studied previously in research about the position of personal computer (PC) displays. Placing a computer display too high or low is known to cause awkward postures of the user and produce neck muscle fatigue and discomfort after a prolonged period of use.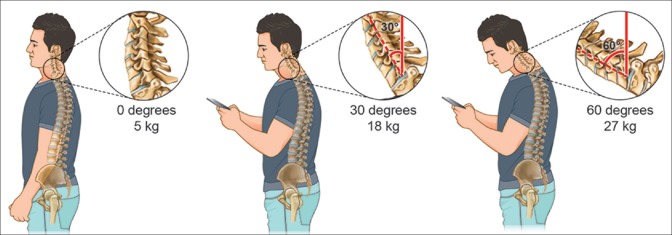 The weight put on the spine dramatically increases when flexing the head forward at varying degrees [Figure]. A full‑grown head weighs 4.54 to 5.44 kg in the neutral position. As the head tilts forward, the forces seen by the neck surges to 12.25 kg at 15°, 18.14 kg at 30°, 22.23 kg at 45°, and 27.22 kg at 60°. The frequent forward flexion causes changes in the cervical spine, curvature, supporting ligaments, tendons, and musculature, as well as the bony segments, commonly causing postural change and pain felt in the neck and other associated areas. The effects of forward flexion of the neck transcend pain to contribute to more associated complications. Often times, the effects of prolonged neck flexion can contribute to nearsightedness, eye strain, or dry eyes, as the eyes are forced to focus on an object placed nearby.
The weight put on the spine dramatically increases when flexing the head forward at varying degrees [Figure]. A full‑grown head weighs 4.54 to 5.44 kg in the neutral position. As the head tilts forward, the forces seen by the neck surges to 12.25 kg at 15°, 18.14 kg at 30°, 22.23 kg at 45°, and 27.22 kg at 60°. The frequent forward flexion causes changes in the cervical spine, curvature, supporting ligaments, tendons, and musculature, as well as the bony segments, commonly causing postural change and pain felt in the neck and other associated areas. The effects of forward flexion of the neck transcend pain to contribute to more associated complications. Often times, the effects of prolonged neck flexion can contribute to nearsightedness, eye strain, or dry eyes, as the eyes are forced to focus on an object placed nearby.What to do
Treating tech neck, also called text neck, typically involves a two-pronged approach:- Improved postural habits
- Manual therapies and stretches
The strategies on this article for treating and/or preventing neck pain while using smartphones also apply to tablets, e-readers, and other handheld devices.
Tips to improve your posture
- Raise the phone. Move the phone (and other devices) up closer to eye level so the head does not have to be tilted forward.
- Take frequent breaks. Spend some time away from the phone—or any type of head-forward posture. If needed, use an alarm or app to set automatic reminders to take breaks from handheld devices.
- Stand up straight. Good posture, with the chin tucked in and shoulders pulled back, keeps the body aligned in a neutral position.
- Exercise regularly. A strong, flexible back and neck are more able to handle extra stress. Some research indicates that teenagers who are active in low-impact team sports or endurance sports are less likely to have neck pain.
In general, finding ways to keep the neck and body more active, rather than hunched over a mobile device, is best for the spine. For example, try scheduling just a few times per day to check text messages and emails, rather than responding multiple times per hour.
Osteopathic treatment
Osteopaths are well equipped to help not only relieve symptoms associated with tech neck, but can also rehabilitate the natural curvature of the spine utilizing Osteopathic treatment. Osteopathic adjustments can help maintain or restore proper biomechanics to the neck and upper back to ensure that the joints remain mobile. Soft tissue mobilization will reduce muscle tension and pain in the neck and upper back and guidance on correct posture and appropriate exercise will help. Osteopathy may also help children grow up aware from a young age how to use technology safely for their physical, emotional and mental health.
Exercise and Stretching
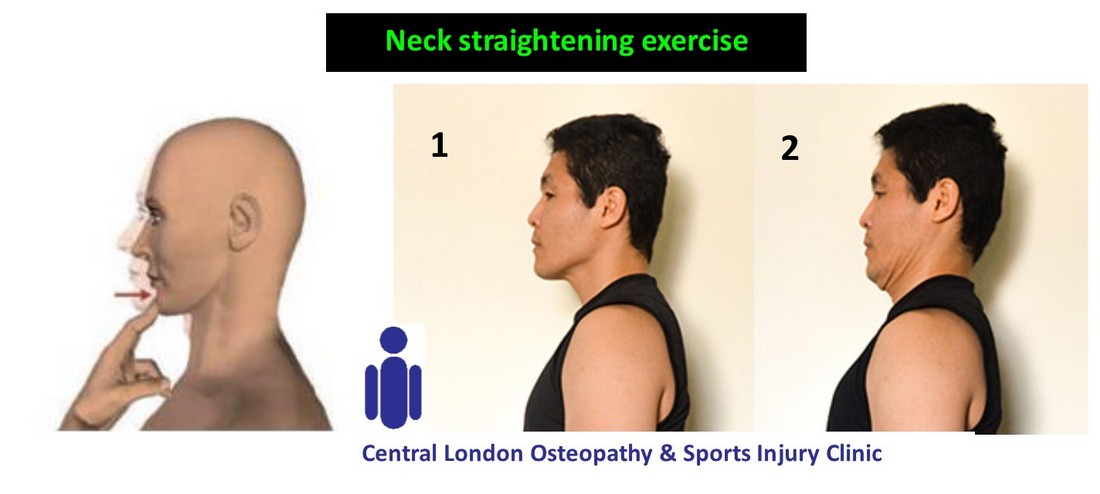
- Ex 1: starting from a natural position, move the head backwards using your chin as a reference point. So, do not bend forward or backwards, just move the whole head/face backwards. Do 15 reps, exhaling when going backwards.
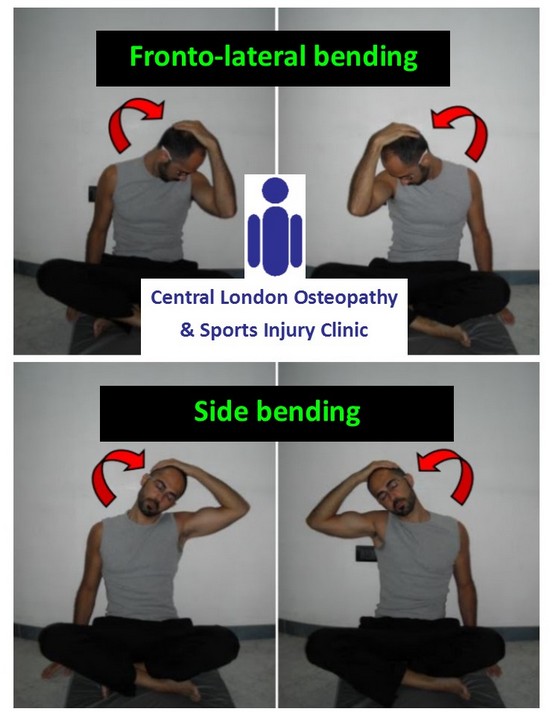
- Stretch 1: (Fronto-lateral bending) bend the head diagonally to one side. Gently hold/push the head forward with the hand of the same side, keeping the other shoulder and arm relaxed. Hold it for 30 sec – 1 min. Do it both sides.
- Stretch 2: (Side bending) side-bend the head to one side. Gently hold/push the head to the side with the hand of the same side, keeping the other shoulder and arm relaxed. Hold it for 30 sec – 1 min. Do it both sides.
Written by Fabio Basile
PLANTAR FASCIITIS: OSTEOPATHIC TREATMENT

Plantar fasciitis is an inflammation that affects the fibrous band from the heel through the entire sole of the foot, to the base of the fingers.
The primary function of the plantar fascia is to support the foot, keeping it in a curved position; if it is too long, the arch of the foot is lowered causing the so-called "flat foot". In addition to this function, the plantar fascia is essential as it acts as a natural shock absorber for the foot, through an adipose cushion that covers it, absorbing the shocks that are generated during normal daily activities. When it becomes inflamed and fails to function, it is called plantar fasciitis. Pain can appear on certain occasions rather than on others, for example when doing sports, standing too much or walking a lot.
Whatever the form of pain, it is good to never neglect plantar fasciitis.
Signs and symptoms
- Pain is most often felt on the sole of the foot and in the arch
- Pain felt when walking and putting weight on the foot
- Pain is often worse in the morning as the band has been in a shortened position for a long period of time while sleeping
- Feeling of tearing on the sole of the foot
- It can often happen after wearing new shoes or bad shoes
Causes
The plantar fasciitis can be caused by several factors:
- age of the patient
- diabetes
- obesity
- standing excessively
- inadequate shoes: they can create tissue problems near the heel (Achilles tendon and heel)
- stress to which the foot is subjected: incorrect exercise can bring stress to the plantar fascia causing inflammation, as well as postural problems.

Osteopathic Treatment
Osteopathy is often fundamental in the treatment of plantar fasciitis. The osteopath will evaluate the mechanics of the affected lower limb, then a general check will follow, which goes from the lumbar, to the pelvis, to the hips down to the tip of the feet.
In addition to this, myofascial structures will be tested and possibly treated, in order to ease the tension that would create an overexertion. A manipulative treatment is also carried out in the area of greater stiffness, both joint and muscular, to restore space between the soft tissues. Dry needling technique, stretching and rolling (tennis ball or specific foam rollers) the plantar fascia is what can bring greater pain relief. Applying ice on site, taking breaks during sports and daily life management are measures that can help accelerate healing.
Sports-related factors
Sports-related injuries are often caused by inadequate training programs - especially overtraining and/or not enough recovery between sessions. Osteopaths are prepared to help you with your training schedule, decreasing the chances of injuries. If you are a runner with plantar fasciitis symptoms, you may also need to monitor your run and identify any deficiencies in your running style that may need to be changed to help treating your problem.
How long will it take to get better?
The condition is variable and can often occur again if the initial cause is still present. The condition often reoccurs in runners and requires constant management and prevention.
Written by Fabio Basile
WORKING FROM HOME:
A COMMON THREAT FOR OUR POSTURE!
 Recently, many office workers are working remotely, using whatever is available in their home to make the workstation as comfortable as possible. However, for a correct setting, good enough to protect our posture, it is crucial to examine some risks and solutions.
Recently, many office workers are working remotely, using whatever is available in their home to make the workstation as comfortable as possible. However, for a correct setting, good enough to protect our posture, it is crucial to examine some risks and solutions.Most of the time people use a normal chair and desk, already existing in their kitchen or dining room, which are usually not adjustable. Moreover, laptops are the most used devices and, again, those can seriously affect the position of the spine, especially neck and shoulders. This happens because the screen is too close to the keyboard, instead it should be high enough to avoid slouching.
What are the RISKS?
 Starting from your body, musculoskeletal problems are the main concern, followed by your mind, such as lack in work efficiency and productivity. Here some example:
Starting from your body, musculoskeletal problems are the main concern, followed by your mind, such as lack in work efficiency and productivity. Here some example:- Neck pain
- Shoulders pain
- Low back pain
- Wrist/Hand pain
- Muscle stiffness
- Headache
- Tiredness
- Vision problems
- Etc
SOLUTIONS
 According to the available budget and the actual situation, one can decide to easily improve the workstation, which in turn will make the posture better, reducing current symptoms. (DO NOT FORGET TO ASK YOUR THERAPIST FOR PROFESSIONAL ADVICES FIRST).
According to the available budget and the actual situation, one can decide to easily improve the workstation, which in turn will make the posture better, reducing current symptoms. (DO NOT FORGET TO ASK YOUR THERAPIST FOR PROFESSIONAL ADVICES FIRST). Here some examples:
- Light: the source of light must be enough and not disturbing, avoiding screen glare
- Feet/Knees: make sure you have enough room for both. Move your table accordingly or whatever is impeding the required space.
- Laptop: position your laptop so that the top of the screen is level with your eye height. To do so, you could simply put your laptop on some boxes/books, or you can use a laptop stand. Laptop stands are STRONGLY RECOMMENDED, because those are usually light, foldable and portable, wherever you work. I recommend NEXSTAND™, a reliable tool, with great reviews. Visit www.nexstand.eu and USE MY DISCOUNT CODE: FABIO10
- Keyboard: an external keyboard is crucial, better if ergonomic. It gives the possibility to raise the laptop screen without creating additional issues to your hands and wrists. It could be purchased with an external mouse, even for a small amount of money.
- Mouse/Touchpad: same as the keyboard, using an external mouse, can make a huge difference. It is also reasonable to consider buying a neutral ergonomic mouse, which allow the hand and wrist to keep a natural and relaxed position. People find often convenient to use the laptop touchpad, although it never ensures a correct posture.
- Lumbar support: neck a lower back pain are quite common, therefore a good spinal support is part of the requirements. Although the neck posture strictly depends on the head and shoulder (hence the above-mentioned recommendations), a lumbar support is was needed to maintain the correct spinal curvatures. If your chair does not have one, try why a towel or a small pillow, positioned between your lumbar spine and the back of your chair.
- Breaks: taking breaks is probably one of the most important things to do. Even if your workstation is properly set, you should not keep the same static posture for more than 30-60 minutes. Hence, 5 minutes break, every regular time intervals, is really helpful. Breaks could often affect the continuity of a task/job so, if you cannot really stop, make sure you have at least 1 break every 2 hours. It could even be quite short, but sure it will be better than nothing!
WHAT TO DO DURING A BREAK? Stand up, shake your legs and upper body, walk if you can, unwind for a few minutes to refresh your mind. A helpful tip is to do 4-5 minutes stretching (roughly 3-4 exercises, to stretch your back, neck and shoulders) See some of those on my social media channels: Instagram video, Youtube video.
Standing desk or workstation
Using your home furniture, you could probably be able to also work standing, positioning your device as previously recommended, such as correct light, laptop position, keyboard, mouse and breaks.
ADDITIONAL TIP: if working standing is doable, try to alternate that with sitting at your desk. A sit-stand adjustable workstation could also be purchased to easily create this perfect setting. Remember that, standing should be predominant, for instance you could stand for 60 minutes, take a small break, and sit for 30 minutes. This helps to avoid static postures for prolonged time.
Written by Fabio Basile
Downloads
click on the file to open or download it